

1- Colorectal Cancer
Information for the patients:
- Overview:
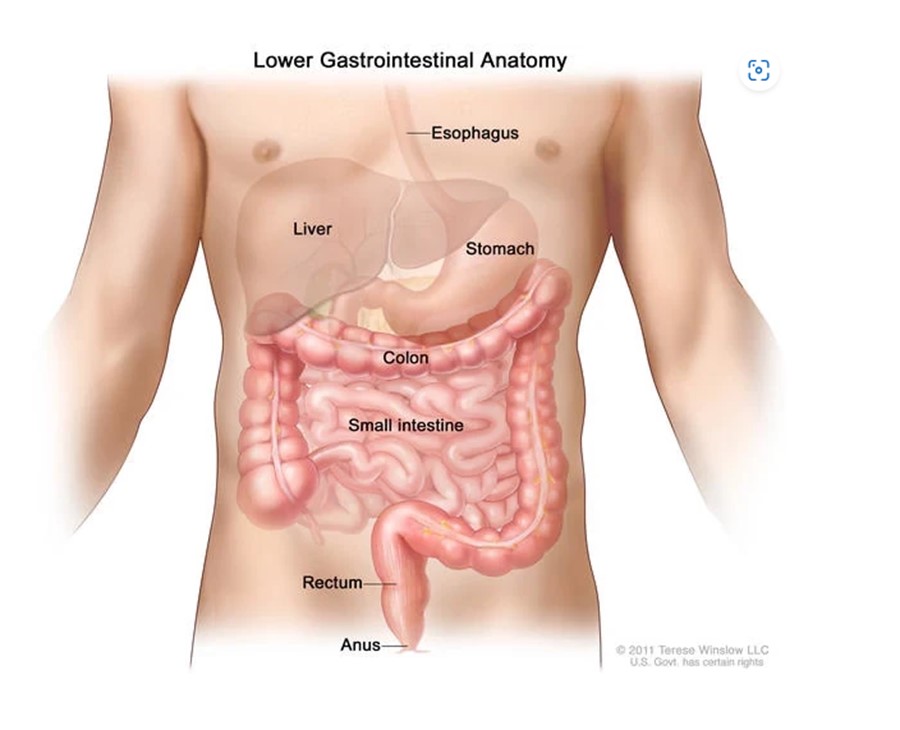
Colon cancer forms in the tissues of the colon, which is part of the large intestine.
The colon is part of the body's digestive system, which is made up of the esophagus, stomach, and the small and large intestines. The first six feet of the large intestine are called the colon. The remaining several inches of the large intestine form the rectum.
Different types of cancer can develop in the colon. Most colon cancers are adenocarcinomas, which are cancers from glandular tissue. Other cancer types that can occur in the colon include
Potential symptoms and signs of colon cancer include:
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors does not mean that you will not get cancer. Risk factors for colon cancer include:
Medical history and physical exam:
Your doctor will ask about your medical history to learn about possible risk factors, including your family history. As part of a physical exam, your doctor will feel your abdomen for masses or enlarged organs, and also examine the rest of your body. You may also have a digital rectal exam (DRE).
Blood tests
Your doctor might also order certain blood tests to help determine if you have colorectal cancer. These tests also can be used to help monitor your disease if you’ve been diagnosed with cancer.
Complete blood count (CBC): This test measures the different types of cells in your blood. It can show if you have anemia (too few red blood cells).
Liver enzymes: You may also have a blood test to check your liver function, because colorectal cancer can spread to the liver.
Tumor markers: Colorectal cancer cells sometimes make substances called tumor markers that can be found in the blood. The most common tumor marker for colorectal cancer is the carcinoembryonic antigen (CEA).
Blood tests for this tumor marker can sometimes suggest someone might have colorectal cancer, but they can’t be used alone to screen for or diagnose cancer. This is because tumor marker levels can sometimes be normal in someone who has cancer and can be abnormal for reasons other than cancer.
Diagnostic colonoscopy
A diagnostic colonoscopy is just like a screening colonoscopy, but it’s done because a person is having symptoms, or because something abnormal was found on another type of screening test.
For this test, the doctor looks at the entire length of the colon and rectum with a colonoscope, a thin, flexible, lighted tube with a small video camera on the end. It is inserted through the anus and into the rectum and the colon. Special instruments can be passed through the colonoscope to biopsy or remove any suspicious-looking areas such as polyps, if needed.
Biopsy
If a suspected colorectal tumor is found during a screening or diagnostic test, it usually is biopsied. In a biopsy, the doctor removes a small piece of tissue with a special instrument passed through the scope. Less often, part of the colon may need to be surgically removed to make the diagnosis.
Imaging tests to look for colorectal cancer and the spread
Computed tomography (CT or CAT) scan
This test can help tell if colorectal cancer has spread to nearby lymph nodes or to your liver, lungs, or other organs.
CT-guided needle biopsy: If a biopsy is needed to check for cancer spread, this test can also be used to guide a biopsy needle into the mass (lump) to get a tissue sample to check for cancer.
Magnetic resonance imaging (MRI) scan: Like CT scans, MRI scans show detailed images of soft tissues in the body. MRI can be used to look at abnormal areas in the liver or the brain and spinal cord that could be cancer spread.
Positron emission tomography (PET) scan
For a PET scan, a slightly radioactive form of sugar (known as FDG) is injected into the blood and collects mainly in cancer cells. PET scans are generally done to help see if the cancer has spread to other parts of the body, outside of the colon or rectum. However, they do not show if cancer has spread to the brain.
The most common treatment for colorectal cancer is surgery to remove the tumor. Chemotherapy and radiation therapy are also frequently involved in plans for therapy. In some cases, a combination of all three will be employed.
Standard treatments include:
Surgery
Surgery (removing the cancerous growth in an operation) is usually the key component of treatment for most patients with colon cancer. It is the most common treatment for people with all stages of colon cancer. Our colorectal surgical team is one of the most experienced in the country.
A surgeon may remove the cancerous growths through:
Chemotherapy
Chemotherapy is a treatment that uses drugs to either kill cancer cells or stop them from growing.
Exciting advances in chemotherapy are allowing patients with advanced disease to get combinations of drugs to shrink tumors, making it easier to take them out later with surgery.
And for cancer that has spread to the liver, we offer leading-edge therapies like hepatic arterial infusion: a small disc implanted under the skin that sends chemotherapy drugs directly into the artery that feeds the liver.
Throughout your treatment, our team of medical oncologists, nurse practitioners, nurses, dietitians, social workers, and other staff will work to minimize the side effects of chemotherapy and maximize your quality of life.
Targeted Therapy:
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells.
Some targeted therapies used in colon cancer focus on certain changes that occur around tumors, specifically the blood supply to tumors. These therapies are called angiogenesis inhibitors, and they stop the growth of new blood vessels that tumors need to grow and spread.
Another kind of targeted therapy for colon cancer attacks a protein on the cell – called the epidermal growth factor receptor (EGFR) - that drives cells to divide and spread.
Immunotherapy
Immunotherapy, also known as biological therapy, uses the body’s own immune system to fight cancer. Cancer cells can trick the immune system so that it does not attack them. Immunotherapy works in a variety of ways to help the immune system spot and destroy colorectal cancer cells.
Radiation Therapy
Our radiation oncologists are national leaders in the use and study of radiation therapy. Radiation therapy uses high-energy x-rays to eliminate cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the cancer. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
While radiation therapy is not as commonly used in colon cancer as in other cancer types, there are times when radiation therapy is recommended:
Colorectal cancer care at Shefa-El Orman:
Our team of experts works together to provide compassionate, comprehensive, and highly coordinated care for patients with colon cancer.
We see about 1,000 cases of colon cancer a year, and offer patients the most advanced treatments, It’s important to note that at Shefa-Orman Hospital there is no one-size-fits-all approach to colorectal cancer. We treat the patient, not the disease, and afford each person the compassion and dignity that everyone deserves. Our nationally renowned physicians will work closely with you and your family to customize your treatment plan according to the characteristics of the disease as well as your own goals, values and preferences.
Multidisciplinary Team: Your team (including gastroenterologists, medical oncologists, radiation oncologists, surgical oncologists, pathologists, radiologists, nurses, social workers, and nutritionists) works together throughout your entire treatment and recovery, ensuring that your care is highly coordinated.
Shefa- Elorman doctors have access to the latest treatment techniques, including:
We offer our patients targeted therapies, advanced surgical procedures, and the full range of nutritional and other support services, from a top-ranked hospital and leading cancer center.
We provide comprehensive services to patients with these cancers, including:
The program includes:
Required documents
Price from: On request
Type of program: Outpatient
Expected duration of the program: 5 days
________________________________________________________________________________
The program includes:
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of previous laboratory tests. After that, you will undergo an additional examination, including laboratory assessment of liver and kidney function. Based on the received results, the doctor will elaborate the chemotherapy regimen. If necessary, related medical specialists will be involved in the elaboration of a treatment regimen (tumor board).
Chemotherapy is carried out as the inpatient procedure or outpatient according to chemotherapy protocol type. After the placement of a venous catheter, you will stay in a comfortable ward. An infusion system will be connected to the catheter, through which the required drug or a drug combination will be administered. All drugs are administered by intravenous drip, slowly, so the total duration of the infusion can be up to several hours. All this time, doctors and nurses will monitor your health condition closely.
After the course of chemotherapy, you will stay under medical supervision in the ward for a few more hours. After the completion of the chemotherapy course and control examinations you will receive the medical report with detailed recommendations regarding further treatment. In the future, you will be able to have a distant consultation with your attending physician and schedule the next course of chemotherapy, if necessary.
Required documents
Price from: On request (regarding chemotherapy protocol)
Type of program: Inpatient or outpatient (regarding chemotherapy protocol)
Expected duration of the program: from 1 to 4 days per cycle (regarding chemotherapy protocol)
______________________________________________________________________________________
The program includes:
How program is carried out
During the first visit, the physician will conduct a clinical examination and go through the results of the available diagnostic tests. After that, you will undergo the necessary additional examinations, such as the assessment of liver and kidney function, abdominal ultrasound scan, CT scan and MRI (if indicated). Based on the results of an additional examination, the physician will clarify the stage of the oncological process, choose the volume of the intervention and the type of anesthesia.
Surgery starts with general anesthesia. After anesthesia, the surgeon makes small incision on the anterior abdominal wall, the doctor litigates large blood vessels and removes the affected areas of the intestine. The surgeon installs drainage into the abdominal cavity and finishes the operation.
After the completion of the operation, you will be transferred back to the ward, under the supervision of the attending physician and nursing staff.
Finally, the attending physician will evaluate the results of control examinations, schedule the date of discharge from the hospital and give you detailed recommendations for further follow-up and treatment.
Required documents
Price from: on request
Type of program: Inpatient
Expected duration of the program: 8 days
_________________________________________________________________________________________
The program includes:
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of previous laboratory tests and instrumental examinations. After that, you will undergo an additional examination, including complete blood count, laboratory assessment of liver and kidney function. Based on the received results, the physician will elaborate the chemotherapy regimen, conduct radiotherapy CT or MRI SIMULATION then planning, make the permanent tattoo marks on the skin to assess the accuracy of the rays and the radiation dose. If necessary, related medical specialists will be involved in the elaboration of a treatment regimen (tumor board).
Chemotherapy and radiation therapy are carried out as the day hospital procedure, without mandatory admission to the hospital. At each visit, the physician will assess your general condition and the marks on the skin. After that, you will be placed in a shielded linear accelerator radiation therapy room.
Each radiation therapy session lasts less than half an hour (including preparation). All this time, doctors and nurses are monitoring your condition, you can communicate with them through a loudspeaker. The procedure is completely painless. Depending on the planned course of treatment, you will visit the hospital from 1 to 3-5 times a week.
Chemotherapy may be through oral or intravenous route according to your treatment plan, during the chemotherapy session, after the placement of a venous catheter, you will stay in a comfortable ward. An infusion system will be connected to the catheter, through which the required drug or a drug combination will be administered. All drugs are administered by intravenous drip, slowly, so the total duration of the infusion can be up to several hours. All this time, doctors and nurses will monitor your health condition closely.
During radiotherapy, you are under close follow-up daily from doctors and nurses.
After the completion of the chemotherapy and radiation therapy course, you will undergo control examinations aimed at assessing your condition and efficacy of treatment. After that you will receive the medical report with detailed recommendations regarding further follow-up and treatment. In the future, you will be able to have a distant consultation with your attending physician and schedule the next course of treatment, if necessary.
Required documents
Price from: on request
Type of program: Outpatient
Expected duration of the program: 39 days
______________________________________________________________________________
مؤسسة شفا الأورمان المُشهره بوزارة التضامن الاجتماعي برقم 5859 لسنة 2016
جميع الحقوق محفوظة مستشفي شفاء الأورمان - صعيد بلا سرطان © 2024