

Overview:
Esophageal cancer is a growth of cells that starts in the esophagus. The esophagus is a long, hollow tube that runs from the throat to the stomach. The esophagus helps move swallowed food from the back of the throat to the stomach to be digested.
Esophageal cancer usually begins in the cells that line the inside of the esophagus. Esophageal cancer can happen anywhere along the esophagus.
Esophageal cancer is more common in men.
Esophageal cancer treatment often involves surgery to remove the cancer. Other treatments may include chemotherapy, radiation or a combination of the two. Targeted therapy and immunotherapy also may be used.
Early on, you could have esophageal cancer with no symptoms. As it advances, symptoms of esophageal cancer may include:
Risk factors for esophageal cancer include conditions and habits that cause irritation in the esophagus. Risk factors may include:
Esophageal cancer diagnosis often begins with imaging tests to look at the esophagus. A sample of tissue may be taken for lab testing.
Barium swallow study
In this test, you will swallow a chalky liquid that contains barium before undergoing an x-ray. The barium will coat the inside lining of your esophagus and appear clearly on the x-ray. This allows your doctor to see any tissue changes.
Upper endoscopy
To see inside the esophagus, a healthcare professional passes the endoscope down the throat and into the esophagus. The health professional looks for signs of cancer.
Biopsy
The health professional removes a very small amount of tissue from the inside of the esophagus. The tissue sample is sent to a lab to look for cancer cells.
Determining the extent of the cancer
After an esophageal cancer diagnosis, you may have other tests to see if the cancer has spread. These tests help your healthcare team find out the extent of your cancer, called the stage. Cancer staging tests often involve imaging tests.
Imaging tests may include bronchoscopy, endoscopic ultrasound, CT, MRI and positron emission tomography scans, also called PET scans. Not every test is right for every person. Talk with your healthcare professional about which tests you will need.
The stages of esophageal cancer range from 0 to 4. A stage 0 esophageal cancer is small and only on the inside surface of the esophagus. As the cancer gets larger and grows deeper into the esophagus, the stages get higher. A stage 4 esophageal cancer has grown beyond the esophagus or has spread to the lymph nodes or other parts of the body.
Treatment:
If you are diagnosed with esophageal cancer, your doctor will discuss the best options to treat it. This depends on several factors, including the type and stage of the cancer and your general health. Your treatment for esophageal cancer will be customized to your particular needs. One or more of the following therapies may be recommended to treat the cancer or help relieve symptoms.
Treatment for early esophageal cancer
Endoscopic mucosal resection (EMR) / Endoscopic submucosal dissection (ESD): Doctors use an endoscope to remove early-stage esophageal cancer that has only invaded the surface of the esophagus. Though these are complex procedures, they are also minimally invasive techniques that do not require any incisions or the removal of the esophagus.
Treatment for locally advanced and advanced cancers
If your cancer has spread to the surrounding tissue or beyond, the following treatments may be used to slow the disease and ease symptoms:
Surgery:
Surgery is the most common treatment for esophageal cancer. To treat more advanced stages of esophageal cancer, surgery may be combined with chemotherapy and/or radiation therapy.
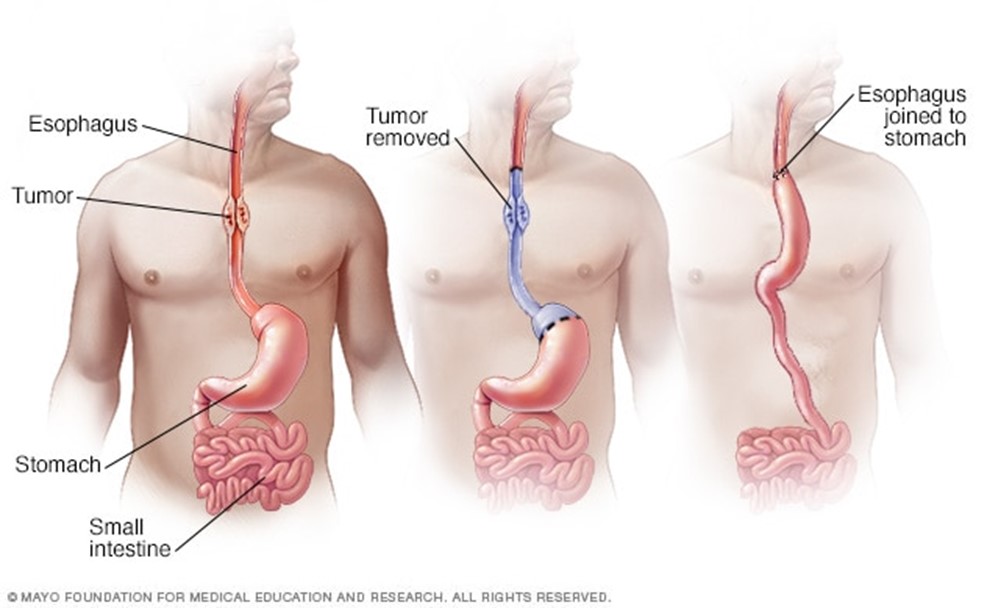
Esophagectomy: Surgery to remove part of the esophagus. During esophagectomy, the surgeon removes the part of the esophagus that contains the cancer and some nearby lymph nodes. The surgeon may also remove some of the upper part of the stomach. When the surgery involves removing some of the esophagus and some of the stomach, it's called an esophagogastrectomy. The remaining esophagus is reconnected to the stomach. Usually, this is done by pulling the stomach up to meet the remaining esophagus. If necessary, part of the colon is used to help join the two.
Surgery to remove the esophagus can be performed as an open procedure using large incisions. Surgery also may be done laparoscopically, where special surgical tools are inserted through several small incisions in the skin. How your surgery is performed depends on your individual situation and how your surgeon wants to approach it.
Chemotherapy:
Chemotherapy works by killing fast-growing cells, including cancer cells. Chemotherapy medicines are typically used before or after surgery in people with esophageal cancer. Chemotherapy can be combined with radiation therapy.
In people with advanced cancer that has spread beyond the esophagus, chemotherapy may be used alone to help relieve symptoms caused by the cancer.
Radiation therapy:
For esophageal cancer, radiation therapy is most often done with a procedure called external beam radiation. During this treatment, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body. Radiation also can be placed inside your body near the cancer.
Radiation therapy is often combined with chemotherapy in people with esophageal cancer. Radiation therapy also is used to relieve complications of advanced esophageal cancer. This may include treating a cancer that grows large enough to stop food from passing to your stomach.
We provides the most advanced radiation treatments for esophageal cancer, including:
Intensity-modulated radiotherapy (IMRT): Radiation beams are delivered at different angles, which are tailored to the specific shape of the tumor.
Immunotherapy:
Immunotherapy recruits the patient’s own immune system in the fight against cancer. For esophageal cancer, patients may be given an immunotherapy known as immune checkpoint inhibitors, which causes the immune system to attack the tumor. Immunotherapy is most commonly used to treat advanced stages of esophageal cancer. It is still being explored in early stages.
Targeted therapies:
Targeted therapy for cancer is a treatment that uses medicines that attack specific chemicals in cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die.
For esophageal cancer, targeted therapy may be combined with chemotherapy for advanced cancers that can't be removed with surgery or for cancers that come back after treatment.
Some targeted therapies only work in people whose cancer cells have certain DNA changes. Your cancer cells may be tested in a lab to see if these medicines might help you.
Treatments for complications:
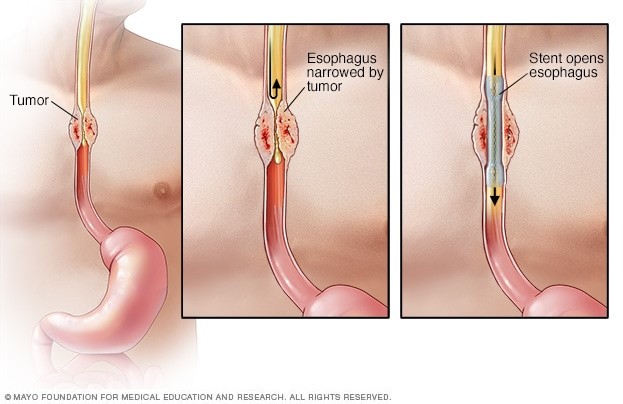
Esophageal stent
Esophageal cancer sometimes grows large enough to narrow the esophagus. It can cause difficulty swallowing. Treatments for this complication can include:
Esophageal stents. Small, expandable metal tubes are placed inside the esophagus with the aid of an endoscope. Once placed, the stent can expand and open up the blocked part of the esophagus, allowing food and liquids to pass through more easily.
Providing nutrition. Your healthcare professional may recommend a feeding tube if you're having trouble swallowing or if you're having esophagus surgery. A feeding tube allows nutrition to be delivered directly to your stomach or small intestine. This gives your esophagus time to heal after cancer treatment.
Palliative care:
Palliative care is a special type of healthcare that helps you feel better when you have a serious illness. If you have cancer, palliative care can help relieve pain and other symptoms. A healthcare team that may include doctors, nurses and other specially trained health professionals provides palliative care. The care team's goal is to improve quality of life for you and your family.
Palliative care specialists work with you, your family and your care team. They provide an extra layer of support while you have cancer treatment. You can have palliative care at the same time as you're getting strong cancer treatments, such as surgery, chemotherapy or radiation therapy.
Your Shefa-El Orman care team
At Shefa-El Orman, experts in several specialties form a multidisciplinary team to care for people with esophageal cancer. Working as a team, doctors are able to provide comprehensive diagnosis and treatment plans that are tailored to your needs. The team includes gastroenterologists, surgeons, pathologists, oncologists, radiologists, radiation oncologists, dietitians, and others as needed.
Shefa-El Orman offers access to the latest esophageal cancer treatments. Our experts are highly experienced in using endoscopic techniques to treat early esophageal cancer and esophageal lesions.
Shefa-El Orman doctors work with you to review all of your treatment options and choose the treatment that best suits your needs and goals.
The range of treatments offered to people with esophageal cancer includes chemotherapy, radiation therapy, targeted therapy, immunotherapy, and minimally invasive and traditional operations, such as esophagectomy.
Shefa-El Orman is dedicated to developing cutting-edge diagnostic tests and innovative treatments for patients with esophageal cancer.
________________________________________________________________________________
The program includes:
Required documents
Price from: On request
Type of program: Outpatient
Expected duration of the program: 5 days
_______________________________________________________________________________
Including: - stent placement in cases of obstruction
The program includes:
Required documents
Price from: on request
Type of program: Inpatient
Expected duration of the program: 5 - 19 days
________________________________________________________________________________
Related to your clinical state and your plan of management
The program includes:
How program is carried out
During the first visit, the doctor will conduct a clinical examination and go through the results of previous laboratory tests and instrumental examinations. After that, you will undergo an additional examination, including complete blood count, laboratory assessment of liver and kidney function. Based on the received results, the physician will elaborate the chemotherapy regimen, conduct radiotherapy CT or MRI SIMULATION then planning, make the permanent tattoo marks on the skin to assess the accuracy of the rays and the radiation dose. If necessary, related medical specialists will be involved in the elaboration of a treatment regimen (tumor board).
Chemotherapy and radiation therapy are carried out as the day hospital procedure, without mandatory admission to the hospital. At each visit, the physician will assess your general condition and the marks on the skin. After that, you will be placed in a shielded linear accelerator radiation therapy room.
Each radiation therapy session lasts less than half an hour (including preparation). All this time, doctors and nurses are monitoring your condition, you can communicate with them through a loudspeaker. The procedure is completely painless. Depending on the planned course of treatment, you will visit the hospital from 1 to 3-5 times a week.
Chemotherapy may be through oral or intravenous route according to your treatment plan, during the chemotherapy session, after the placement of a venous catheter, you will stay in a comfortable ward. An infusion system will be connected to the catheter, through which the required drug or a drug combination will be administered. All drugs are administered by intravenous drip, slowly, so the total duration of the infusion can be up to several hours. All this time, doctors and nurses will monitor your health condition closely.
During radiotherapy, you are under close follow-up daily from doctors and nurses.
After the completion of the chemotherapy and radiation therapy course, you will undergo control examinations aimed at assessing your condition and efficacy of treatment. After that you will receive the medical report with detailed recommendations regarding further follow-up and treatment. In the future, you will be able to have a distant consultation with your attending physician and schedule the next course of treatment, if necessary.
Required documents
Price from: on request
Type of program: Outpatient
Expected duration of the program: 39 days
___________________________________________________________________________________
The program includes:
Required documents
Price from: on request according to treatment protocol
Type of program: Inpatient or outpatient depending on chemotherapy protocol
Expected duration of the program: 5 days
مؤسسة شفا الأورمان المُشهره بوزارة التضامن الاجتماعي برقم 5859 لسنة 2016
جميع الحقوق محفوظة مستشفي شفاء الأورمان - صعيد بلا سرطان © 2024